There are a variety of treatments available for the narrowed or blocked blood vessels that cause peripheral artery disease (PAD). The most commonly utilized PAD treatments include bypass graft surgery in the leg and minimally invasive options such as angioplasty, stenting, and atherectomy. When comparing PAD treatments, it’s important to keep in mind that determining the best option for each patient depends on the severity of your peripheral artery disease and the location of the blockage. A PAD specialist will determine the best options available for you only after diagnosis and thorough examination. But you can start to educate yourself on your options here.
Bypass Graft Surgery in the Leg
Bypass graft surgery involves the removal of a healthy blood vessel, typically the saphenous vein in the leg, and grafting it above and below the site of the blockage. The procedure ultimately allows blood flow to “bypass” the blocked area. You should note that this type of surgery might be the only option available in advanced PAD cases — often in these advanced cases, every effort is being made to save patients from amputation or permanent disability, so a more aggressive treatment may be appropriate. Bypass graft surgery is a well-established procedure that when successful, can result in drastically reduced risk of both amputation and death. This surgery can be used when a patient is not a candidate for minimally invasive surgery, or after minimally invasive techniques have failed.
Bypass graft surgery is major surgery that requires general anesthesia (epidural/spinal), a hospital stay ranging from 3-10 days, and sometimes assistance from a medical professional or aide after returning home. Multiple incisions are necessary to remove the new blood vessel for grafting, and to access the affected blood vessel both above and below the site of blockage. Incision sites require more stitches or staples, increasing the risk of infection.There is a potential for grafted blood vessel to fail, due to a technical error, an abnormal narrowing or blockage at the graft site, or progression of peripheral artery disease. There are also common complaints of leg swelling that causes discomfort. This can resolve with time, or remain a persistent complaint. The expense can be far greater when compared to minimally invasive surgeries, due to the increased hospital stay and in-home care that is often required.
All of the above are reasons why the need for early diagnosis of PAD is stressed, because early diagnosis can often allow for minimally invasive options to be considered.
Minimally Invasive Procedures
Angioplasties, stenting, and atherectomies are procedures that use catheterization (insertion of a small specialized tube) through a small incision site to access and remove or open a blockage in a blood vessel.
An angioplasty accomplishes this through insertion and inflation of a balloon through the catheter into the blocked or narrowed vessel, compressing the plaque buildup against the vessel walls. These balloons are sometimes coated with medications that reduce the risk of restenosis, a recurrence of the blood vessel narrowing.
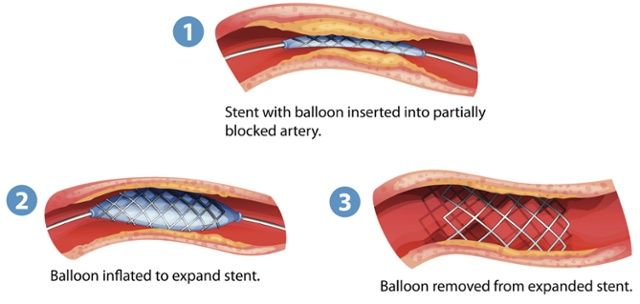
Stenting involves the insertion of an expandable metal or plastic scaffold to hold the vessel open. Stents are frequently used in combination with the angioplasty balloon. The balloon is expanded sufficiently to allow the stent, which is mounted on the balloon, to open the vessel. Once the expansion is complete, the balloon is deflated and removed leaving the stent in place.
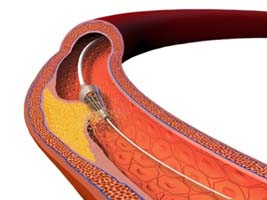 Atherectomies utilize a sharpened tip, grinding bit, or laser to remove hardened blockages in blood vessels. These tips scrape, vacuum, or vaporize plaque, making atherectomy the only technique which physically removes plaque from the artery.
Atherectomies utilize a sharpened tip, grinding bit, or laser to remove hardened blockages in blood vessels. These tips scrape, vacuum, or vaporize plaque, making atherectomy the only technique which physically removes plaque from the artery.
These techniques are frequently used in combination with one another, depending on patient needs and physician recommendations.
Advantages of Minimally Invasive Techniques
- Minimally invasive techniques can be performed on an outpatient basis with a quick return to normal activities.
- Major complications uncommon.[i]
- Only local anesthesia needed.
- While outcomes are the same as in surgery, there is an economic component in that minimally invasive techniques are significantly less expensive.[i]
Possible Risks include
- Risk of bleeding, clotting, and infection at the catheter insertion site – though far less of a risk than in bypass graft surgery.
- Potential for the same artery to become blocked again, since an alternative route for blood to flow is not created, as in surgery.
- Rarely, balloons, stents, or catheter tips used in surgery can potentially perforate or tear the arterial wall, damaging the blood vessel beyond repair and requiring emergency bypass surgery.
- Debris dislodged while attempting to remove plaque could cause an embolus (blockage) that lodges in another blood vessel.
- Blockage can return gradually over time, eventually requiring surgery.
What To Think About
Bypass graft surgery is a surgical technique proven to reduce risk of amputations and death in patients with advanced peripheral artery disease. However, when it is an appropriate option, minimally invasive procedures are generally preferred by both physicians and patients. These less invasive interventions are beneficial due to their cost effectiveness, short recovery times, and minimal risk of complications. A PAD specialist will be able to assess your prognosis and recommend the best treatment available for you. Again, minimally invasive procedures may not be an option if diagnosis of PAD is delayed. Talking to your doctor at the first signs and symptoms of the disease can help prevent long hospital stays and expensive medical bills that often accompany bypass graft surgery in treatment for PAD. You can educate yourself before seeing your doctor with our 11 Questions to ask Your Doctor about PAD article.
Sources:
[i] http://www.webmd.com/heart-disease/angioplasty-for-peripheral-arterial-disease-of-the-legs