Peripheral artery disease (PAD) is a narrowing or blockage of the blood vessels (arteries) with deposits called plaque. This blockage can result in pain, discomfort, and numbness in the extremities, usually the legs. One of the most important steps after a diagnosis is to search for a PAD specialist immediately, as blockages, and potentially pain, will worsen over time and can become life threatening if left untreated.
Many PAD treatment options are available, and you should fully discuss each with a PAD specialist. A physician who is a PAD specialist will guide you in selecting the best option for treating your symptoms, depending on the location and severity of your blockage. One treatment option may be atherectomy.
What is An Atherectomy?
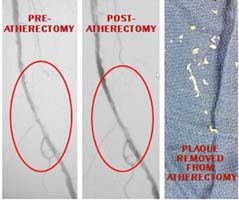
 Atherectomy is a method used to remove plaque from the blood vessels. Because it cleans out the “drainage pipes” of the body, it’s sometimes referred to as the “Roto-rooter” procedure. This procedure is performed in an outpatient setting, generally in the catheterization, or “cath” laboratory, by a trained vascular surgeon or interventional radiologist.
Atherectomy is a method used to remove plaque from the blood vessels. Because it cleans out the “drainage pipes” of the body, it’s sometimes referred to as the “Roto-rooter” procedure. This procedure is performed in an outpatient setting, generally in the catheterization, or “cath” laboratory, by a trained vascular surgeon or interventional radiologist.
What Are the Benefits of An Atherectomy?
- Atherectomy carries the same minimal risks as other minimally invasive procedures; however, it is the only technique that actually removes plaque from the vessel.
- Studies have shown no major difference in patient outcomes when atherectomy and angioplasty are compared.
- Patients are at no greater risk of reoccurrence of blockage, amputations, or death following either procedure.[i] This holds true even for patients with pre-existing conditions, such as diabetes, who have shown no increased risk of complications or blockage reoccurrence when atherectomy is used in place of, or in addition to, angioplasty and stenting.[ii]
- Atherectomies are useful at removing highly calcified plaques, which are too hardened to be crushed into the wall with either the angioplasty balloons or stenting devices.
Are There Any Disadvantages To An Atherectomy?
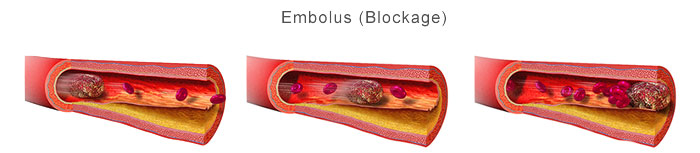
- There is a risk of an embolus (blockage) forming from the dislodged debris following atherectomy. Care is taken to remove all debris during the procedure, and careful monitoring occurs afterwards to ensure that this does not occur.
- Rarely, perforation of the blood vessels with the atherectomy device during the procedure may require emergency bypass to repair.
- Atherectomy is not a guaranteed life-long repair. Lifestyle modifications and medication may be required, as blockages can return
What Should I Expect?
After pre-procedure testing confirms that you are a good candidate for an atherectomy, a procedure will be scheduled.
The Night Before…
- Like most interventional procedures, your physician will generally recommend fasting beforehand. A light, early dinner, followed by a fast after midnight is the typical protocol.
When You Arrive At the Outpatient Center…
- When you arrive at the outpatient center, consent forms will need to be signed to allow for emergency interventions if needed.
- The area where the catheter will be inserted (the groin, the foot, or the arm) will be washed and shaved to prevent infection.
As the Procedure Begins…
 A mild sedative will be given through an IV. The area selected for catheter insertion will be numbed with a local anesthetic. Some patients report feeling pressure or pushing sensations while the procedure is conducted, but typically no pain is reported.
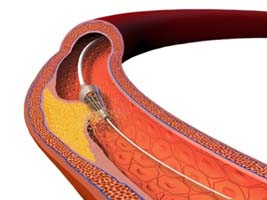
A mild sedative will be given through an IV. The area selected for catheter insertion will be numbed with a local anesthetic. Some patients report feeling pressure or pushing sensations while the procedure is conducted, but typically no pain is reported.- Then, the catheter will be inserted into the blood vessel and guided to the blockage. A contrast medication (a special type of dye) may be injected to assist with visualization of the area to be treated. Depending on the type of catheter, a sharpened tip, grinding bit, or laser will remove the plaque by scraping, grinding, or vaporizing. Either a chamber underneath the catheter or a suction device will remove the blockage from the body.
- Multiple insertions may be required to completely remove the blockage.
- Ultrasounds are used to see the blockage site and ensure that as much plaque as possible is removed.
- Most atherectomy devices are set up to automatically capture any dislodged debris that may occur during the procedure.
To Conclude the Procedure…
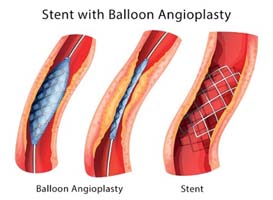 Once blood flow is restored, angioplasty and/or stenting might be performed to protect against future blockages.
Once blood flow is restored, angioplasty and/or stenting might be performed to protect against future blockages.- During angioplasty, a balloon is inflated at the area of blockage, flattening any remaining plaque against the blood vessel wall.
- Stents are mesh-like metal tubes that are inserted in a collapsed form, and spring open once inserted into the area of the previous blockage, holding the vessel open.
- After stent insertion, the catheter is removed and the insertion site may be closed with stitches.
- The procedure itself will generally take 1 – 3 hours.
RELATED: What is Angioplasty?
After the Procedure…
- Patients will have to gradually increase mobility, initially lying flat for a few hours, then sitting up, then walking between 6 – 24 hours after the procedure.
- Normal activity can typically be resumed within 24 – 48 hours.
Why Would Your Physician Recommend An Atherectomy?
There are many benefits to choosing an atherectomy as treatment for peripheral artery disease. Atherectomies are especially recommended when angioplasty and stenting are not possible. This can occur when the blockage is in a particularly difficult to reach location, or is too hardened or severe to be flattened with the angioplasty balloon or stent device alone. Because it scrapes away these difficult to reach, hardened plaques, atherectomy is frequently used as a preliminary step prior to angioplasty or stenting.
To determine if you’re a good candidate for atherectomy, you should search for an interventional radiologist or vascular surgeon in your area that specializes in treating PAD to discuss your diagnosis and potential treatment. PAD treatment options vary based on the specifics of your individual case, and it’s important to begin treatment as soon as possible.
UP NEXT: Comparing PAD Treatments: Minimally Invasive vs Bypass Graft Surgery
Sources:
[i] http://www.ncbi.nlm.nih.gov.proxy.lib.mcw.edu/pubmed/23755978
[ii] http://www.ncbi.nlm.nih.gov/pubmed/26250748