Have you lost your sex drive, feeling irritable and fatigued, or having trouble sleeping? These could be symptoms of low testosterone, and varicoceles might be to blame.
Men diagnosed with varicoceles can experience various symptoms that include pain, testicular atrophy and in some, a varicocele causes low testosterone levels.
Want to learn more? Let’s look more in depth at what a varicocele is and explore the link between varicoceles and low testosterone.
The Basics of Varicoceles
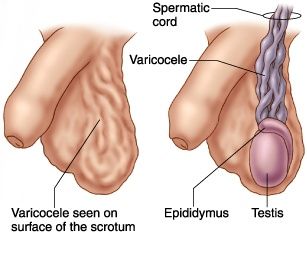
So, what is a varicocele? If you have one, you’re not alone. One out of 10 men suffer from varicoceles. Varicoceles occur when the veins in the scrotum (the sack that holds your testicles in place) become enlarged. Veins have one-way valves, and when they’re faulty, blood can begin to pool in the scrotum, causing the veins to become enlarged. These enlarged veins are called a varicocele.
What is Testosterone?
Testosterone is a hormone that’s produced in your testicles. Testosterone stimulates the development of male characteristics and plays a key role during puberty. It regulates growth spurts in boys, growth of pubic hair and genital changes during puberty.
Symptoms of Low Testosterone

Low testosterone can cause many symptoms in men. While some of these symptoms can be just mildly unpleasant, others can be more serious. Some common symptoms of low testosterone are:
- Decreased libido, or sex drive
- Decreased muscle mass
- Depression
- Fatigue
- Hot flashes
- Inability to concentrate
- Inability to continue to exercise at usual levels
- Increased body fat
- Irritability or crankiness
- Issues with sleep
- Lack of ambition
- Lack of energy
- Loss of hair and deteriorating nails
- Reduction in bone mineral density, or thin bones
- Sexual dysfunction, including inability to sustain or maintain an erection i
Can a Varicocele Cause Low Testosterone?
Some studies have shown that a varicocele causes low testosterone levels. In one recent study, the testosterone levels of 325 men with varicoceles were compared with the levels in 510 men who did not have varicoceles. The results showed that regardless of age, the men with varicoceles had significantly lower testosterone levels than the men without them. ii
What Are Your Options if You Have Low Testosterone?
If you’re experiencing any signs or symptoms that may be related to a low testosterone level, talk to your doctor about the options available for treatment. You’ll likely want to treat your varicocele if it’s interfering with your testosterone production.
There are two main options for varicocele treatment: varicocele surgery (a.k.a. varicocelectomy) or the minimally invasive procedure known as varicocele embolization.
Several surgical approaches can be used to close off the faulty veins to correct the varicocele. These include open surgery, microsurgery and laparoscopic surgery. There are some important differences to note with each procedure.
Open surgery – a surgeon makes an incision into either the upper scrotum, the groin, or the lower abdomen, finds the faulty veins, and ties them off so blood can’t flow through them. Open surgery requires either general or local anesthesia. With this approach, there is a higher rate of the varicocele recurring.
Microsurgery – a complex surgery performed using a microscope. The surgeon can more easily identify the exact veins. While the procedure is more complex, it has less complications and a lower recurrence rate than the open surgical approach. This approach has a lower rate of recurrence, but it is still a technically complex procedure.
Laparoscopic – the surgery is performed through small incisions and uses specific surgical instruments to see inside the body and make the repairs. The laparoscopic approach requires patients to undergo general anesthesia, and higher complication rates are associated with it than with other procedures.
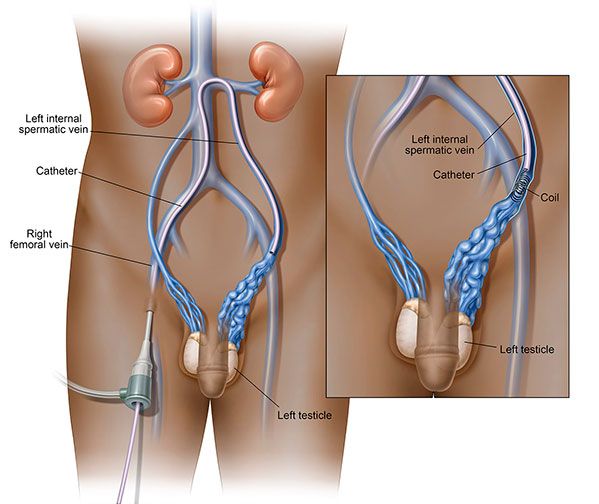
Varicocele embolization is a minimally invasive procedure that can be safely performed on an outpatient basis. The procedure lasts about one to two hours, and you are given a mild sedation and a local anesthesia.
During varicocele embolization, a small nick is made, typically in the groin area. Then, using x-ray guidance, a small tube called a catheter is threaded into your femoral vein and advanced to the site of your varicocele. Once inside your varicocele, a special solution along with a small metal coil (or coils) is directed through the catheter into the affected vein(s) to stop the flow of blood to the varicocele. This results in the blood flow being redirected to nearby healthy scrotal veins and back toward your heart.
Embolization is often the Preferred Treatment for a Varicocele
While both surgical ligation and varicocele embolization are considered 90% successful, more men who have undergone both embolization and surgical litigation prefer the varicocele embolization treatment to surgery. Just like with surgical ligation, varicocele embolization can cause a rise in testosterone and other important fertility biomarkers. iii
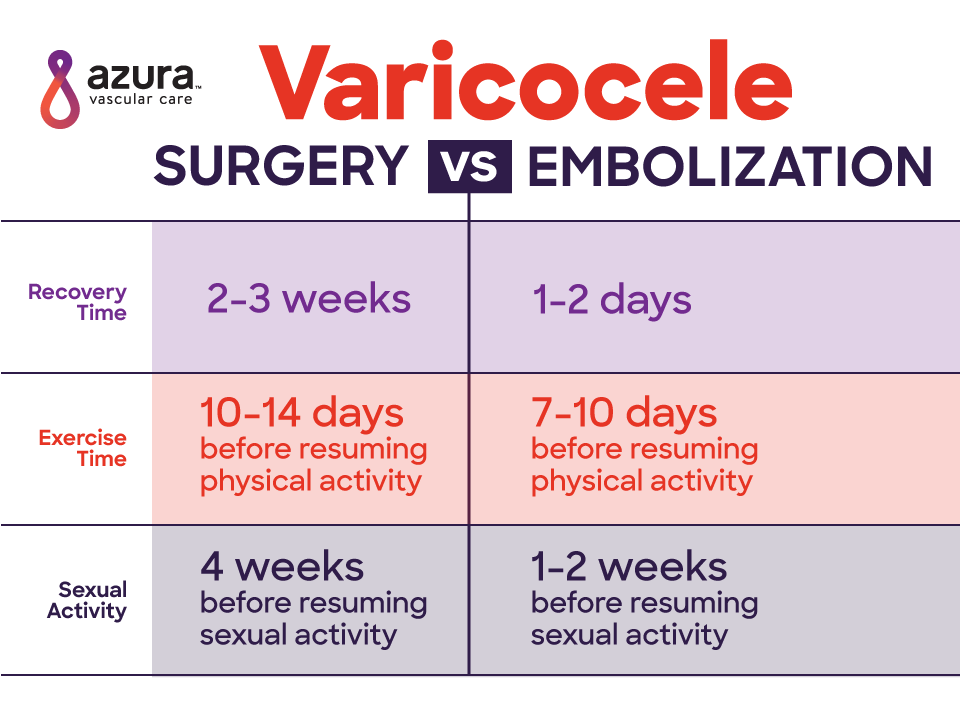
Moreover, many men feel that varicocele embolization has several important advantages over varicocele ligation surgery, including:
- The recovery time is faster with embolization
- You can get back to exercising earlier than you can with surgery
- You can return to normal sexual activity sooner after varicocele embolization
If you’re experiencing symptoms related to low testosterone, especially if you’ve also been diagnosed with or think you may have a varicocele, talk to your doctor today about your potential treatment options.
Sources:
i Mayo Clinic (2017) Varicoceles. Retrieved from: http://www.mayoclinic.org/diseases-conditions/varicocele/basics/treatment/con-20024164
ii C. Tanrikut, M. Goldstein, J. S. Rosoff, R. K. Lee, C. J. Nelson, and J. P. Mulhall. (2011). Varicocele as a risk factor for androgen deficiency and effect of repair. BJU International, DOI: 10.1111/j.1464-410X.2010.10030.x
iii J. Prasivoravong, F. Marcelli, L. Lemaitre, P. Pigny, N. Ramdane, M. Peers, V. Mitchell, and J. Rigot. Beneficial effects of varicocele embolization on semen parameters. Basic. Clin. Androl. 2014, 24(9). DOI 10.1186/2051-4190-24-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4349315/