If you are starting hemodialysis as a treatment for kidney failure, you will need one of three types of dialysis accesses to make hemodialysis possible:
All three types provide access to your blood which is needed for your regularly scheduled hemodialysis sessions, but there are differences between them. Learn how each type is placed, how best to maintain it, and potential complications to watch out for.
The Types of Arteriovenous (AV) Access for Hemodialysis
The term arteriovenous refers to the connection between an artery and a vein. You may remember from biology class that arteries are the blood vessels that carry oxygenated blood from your heart to all parts of your body and veins carry de-oxygenated blood back to your heart.
An AV access is surgically created by making a direct connection between an artery and a vein which bypasses the capillaries. Normally, arteries and veins are not directly connected. There are two types of AV accesses: an AV fistula and an AV graft.
AV Fistula
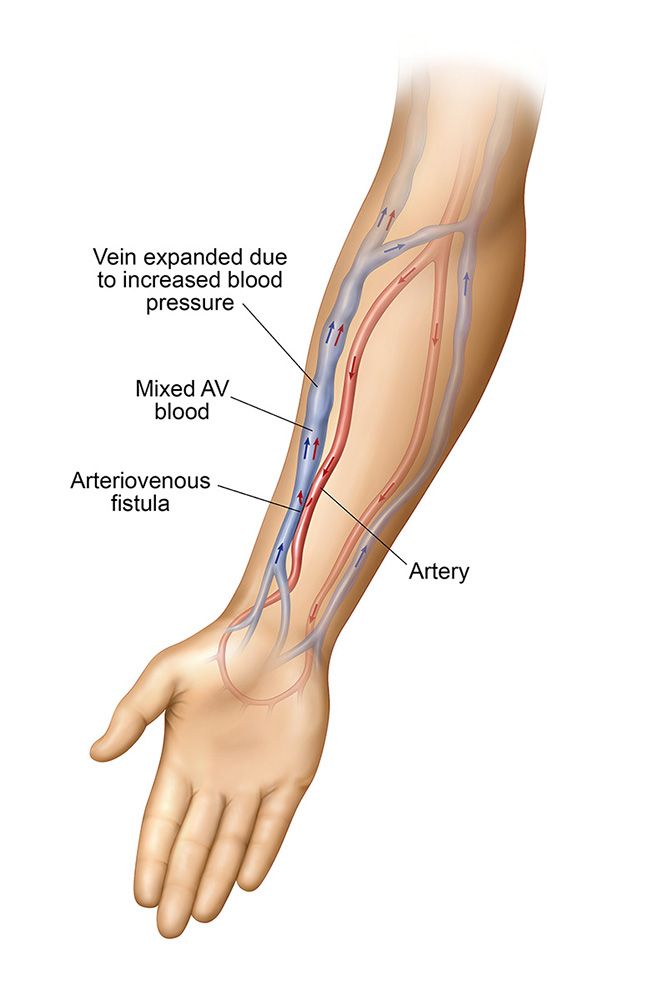 The AV fistula is created from your own vessels because a vein doesn’t normally have a strong blood flow, and is not large enough to accommodate the needles required for accessing the blood so it would not provide adequate hemodialysis treatments. A connection is made between your artery and vein resulting in the enlargement of the vein which allows for your dialysis care team to successfully place the needles used for dialysis.
The AV fistula is created from your own vessels because a vein doesn’t normally have a strong blood flow, and is not large enough to accommodate the needles required for accessing the blood so it would not provide adequate hemodialysis treatments. A connection is made between your artery and vein resulting in the enlargement of the vein which allows for your dialysis care team to successfully place the needles used for dialysis.
The AV fistula is created from your own vessels because a vein doesn’t normally have a strong blood flow, and is not large enough to accommodate the needles required for accessing the blood so it would not provide adequate hemodialysis treatments. An artery is a larger, deeper blood vessel with a very high flow. In addition an artery has stiff, rigid walls which are more difficult to access with needles. It is for these reasons that the connection is made between your artery and vein resulting in the enlargement of the vein which allows for your dialysis care team to successfully place the needles used for dialysis.
The additional volume of blood flowing into the vein from the artery causes the vein to become enlarged. The vein walls grow stronger to support the increased pressure and volume of blood. At this point, the AV fistula has been created and can now develop and mature in order for it to be used for dialysis.
The AV fistula is considered by physicians to be the preferred type of dialysis access because it lasts longer, performs better, and is less likely to become infected or clotted.
Possible Complications Associated with an AV Fistula
Sometimes the artery diverts too much blood into the vein, and not enough goes to your hand and fingers. This is known as Steal Syndrome and can cause your hand to feel cold. A vascular specialist may need to limit some of the blood flowing into the fistula to allow more blood to flow to the hand. This procedure is known as “banding.”
With repeated use during hemodialysis, scar tissue can develop inside an AV fistula. Scar tissue blocks the path of the blood flow, clogging the AV fistula. Your vascular specialist will perform an angioplasty; a procedure that moves scar tissue out of the way with a special balloon-tipped catheter. Maintaining adequate flow through your AV fistula may require occasional angioplasty procedures. [1]
AV Fistula Maintenance
Whether you have an AV fistula or an AV graft, you need to take care of your AV arm. Avoid overuse or excessive pressure for as long as you use the fistula or graft. Staying healthy is important too because an infection can occur more easily if you have a weakened immune system. To protect your access, it’s best to not allow anyone to draw blood, insert an IV or take blood pressure on your access arm.
With proper care, an AV fistula can last for years. Maintaining your AV fistula requires daily checks to ensure that it is working properly. The dialysis center staff will teach you how to check your AV fistula. Because of the high-pressure blood flow through the AV fistula, you will feel a rapid vibration through the skin over the AV fistula area. This feeling, known as a “thrill,” indicates that the fistula is working.
RELATED: What Does a Health AV Fistula Look Like?
Arteriovenous (AV) Graft
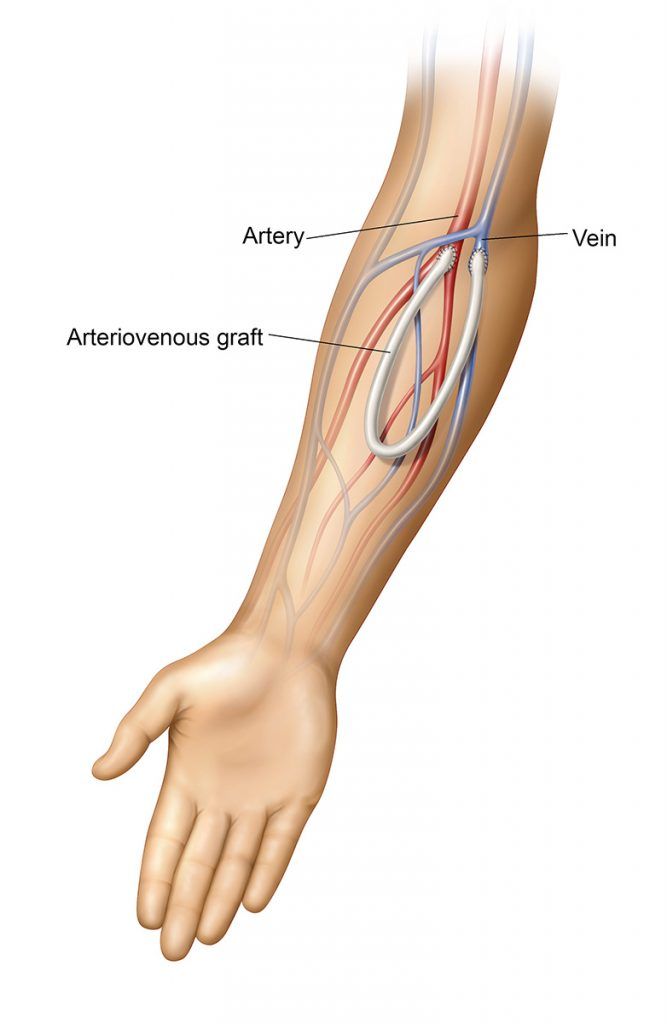 An AV graft is an option for patients whose veins are very small and most likely won’t mature into a working fistula. A surgeon will connect a soft, biocompatible flexible tube between an artery and a vein beneath your skin. Blood from the artery flows through the AV graft and then into the vein. This creates an area on your arm suitable for hemodialysis because the AV graft material is strong enough to use repeatedly. An AV graft usually takes less time to be ready for use than it does for an AV fistula to mature. Most AV grafts can be used for dialysis treatment a few weeks after placement.
An AV graft is an option for patients whose veins are very small and most likely won’t mature into a working fistula. A surgeon will connect a soft, biocompatible flexible tube between an artery and a vein beneath your skin. Blood from the artery flows through the AV graft and then into the vein. This creates an area on your arm suitable for hemodialysis because the AV graft material is strong enough to use repeatedly. An AV graft usually takes less time to be ready for use than it does for an AV fistula to mature. Most AV grafts can be used for dialysis treatment a few weeks after placement.
Although the infection and complication rates are higher than compared to an AV fistula, the AV graft has advantages over the other hemodialysis access types. Because an AV graft is placed completely under the skin, the infection rate is much lower than with a catheter. AV grafts may also last longer than catheters.
Possible Complications Associated with an AV Graft
AV grafts have a higher rate of infection than AV fistulas because they are made of an artificial material. Germs bind more easily to artificial materials than to the body’s own tissue. AV grafts can become infected when germs enter through the dialysis needle sites and grow on the AV graft material.
Scar tissue can build up inside an AV graft, just like it does inside an AV fistula. Each time the dialysis needles are removed, scar tissue forms to seal the holes in the skin. The vascular specialist will also use angioplasty to move the scar tissue out of the way. Anything that presses too hard on the AV graft, like tight clothing or jewelry, can compress it and slow the blood flow. Large blood clots can form inside the AV graft if the blood flow is too slow. This may make the AV graft difficult or impossible to re-open.
AV Graft Maintenance
AV grafts require the same daily maintenance as AV fistulas. You will need to feel for the thrill and wash the skin over the AV graft regularly. AV grafts may also require angioplasty procedures to keep them working well. [2] The AV graft material may wear out over time, requiring placement of a new AV graft.
Central Venous Catheter (CVC)
 Because an AV fistula needs time to mature, it is not an option for someone who needs to start hemodialysis right away. If you need to start hemodialysis urgently, your only option is a CVC to begin treatment. An AV fistula can be created and given time to mature while a CVC is being used.
Because an AV fistula needs time to mature, it is not an option for someone who needs to start hemodialysis right away. If you need to start hemodialysis urgently, your only option is a CVC to begin treatment. An AV fistula can be created and given time to mature while a CVC is being used.
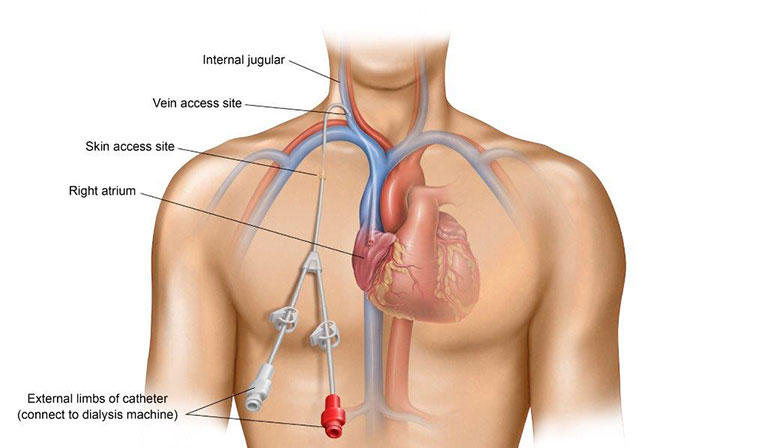
A CVC is a flexible tube that is placed through the skin in your neck, chest or groin. This allows immediate access to your blood for hemodialysis without waiting for an AV fistula to mature or for an AV graft to heal. A CVC stays in place for repeated use instead of being inserted with each dialysis session.
The CVC does not make a connection between your artery and a vein. The catheter is inserted through a large vein in your chest and the tip of the catheter rests in the upper right chamber of your heart. Because the catheter is partly external and partly internal, germs on the skin’s surface can travel along the catheter and into the bloodstream causing infection. A bloodstream infection is a serious, sometimes lethal, complication.
CVC Maintenance
It’s important that you take very good care of your CVC, making sure that it stays clean and dry to limit the risk of infection. Be aware that with a CVC, you cannot shower or swim. The CVC also should be secure to prevent it from becoming displaced. The dressing over the catheter site should be changed at every treatment.
Potential Complications Associated with a CVC
Central venous catheters can potentially cause damage to central veins, including injury, bleeding and hematoma (a collection of blood that accumulates in the tissue around the injured blood vessel) during CVC placement. Damage to and stenosis of the central veins may limit future access sites.
CVCs can become clogged. Fibrin sheathing can block the internal catheter tip. This occurs when clotting factors in the blood build up inside and/or around the catheter. Although there are medications that may help dissolve the clots, a new catheter may be needed to continue hemodialysis.[3]
If you have a CVC, infection is a serious potential complication. An infection can lead to shock or even death. If it’s suspected you might have a CVC infection, blood cultures will be drawn from separate sites and antibiotics will be prescribed.
A CVC is not recommended for most people as a permanent method to provide hemodialysis access due to the potentially serious central venous catheter complications that can arise. However, for those needing immediate access, a CVC may be the best option – even if it’s a temporary solution.
RELATED: 5 Common Central Venous Catheter (CVC) Complications
Putting it all together
Learning as much as you can about your hemodialysis access, including the placement procedure, required maintenance, and complications to be on the lookout for, can help you navigate the lifesaving process of dialysis and live your best life.
Sources:
(1) Elias, Nahel, and Stapleton, Sahel. Arteriovenous Fistula Creation. Journal of Medical Insight. https://jomi.com/article/110/arteriovenous-fistula-creation
(2) Al-Jaishi, Ahmed A., Liu, Aiden R., Lok, Charmaine E., Zhang, Joyce C., and Moist, Louise M., 2017. Complications of the Arteriovenous Fistula: A Systematic Review. JASN June 2017, 28 (6) 1839-1850; DOI: https://doi.org/10.1681/ASN.2016040412
(3) Kornbau, Craig, Lee, Kathryn C., Hughes, Gwendolyn D., and Firstenberg, Michael S., 2015. Central line complications. Int J Crit Illn Inj Sci. 2015 Jul-Sep; 5(3): 170–178. doi: 10.4103/2229-5151.164940


