Maturation failure, risk of infection, and scars are common concerns for surgically-created fistulas, but the techniques now being utilized in percutaneous fistula creation help to minimize and eliminate some of those concerns for patients.
If you are nearing end-stage renal disease and may require hemodialysis treatment, this article discusses your potential options for fistula creation, the advantages and disadvantages of percutaneous fistula creation, and if a percutaneous fistula is right for you.
Percutaneous Fistula Creation vs. Surgical Fistula Creation
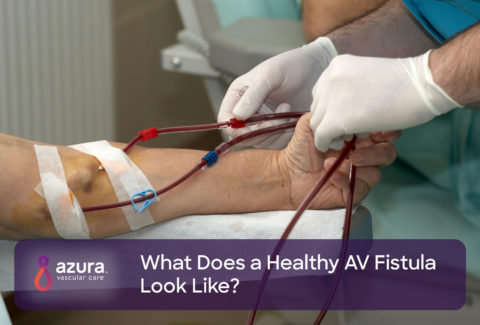
A fistula is a connection created between an artery and a vein, usually in the arm, that will serve as vascular access during dialysis treatment. Vascular access is a way to reach the blood for hemodialysis. The access allows blood to travel through blood lines to the dialysis machine where it is cleaned by a special filter and the returned to your body. (i)
Traditionally, vascular specialists or vascular surgeons have created fistulas through minor surgery. An incision is made in the arm, called an “open-approach,” and the surgeon or specialist will identify the vessels, create the AV fistula by suturing the artery and vein together, and finally suture the skin closed. (ii) The suture or clips in the wound will remain in place for 7-10 days and will then be removed.
The word percutaneous pertains to any medical procedure where access to inner tissues or vessels is done via needle-puncture of the skin, rather than opening the skin as in traditional surgical methods. Utilization of a percutaneous fistula creation method, a special device is used to create the fistula by introducing and passing a wire and catheter within the vessels, so there is no need for an incision, nor is there any disruption of the surrounding tissues. (iii)
Currently, there are two technologies available regarding percutaneous fistula creation.
Types of Percutaneous Fistula Creation
Both methods currently available for percutaneous fistula creation are designed around the vascular anatomy in the upper forearm. Similar to the surgical creation of an AV fistula, it is imperative that the patient first has an ultrasound completed in order to map the vessels of the arm and determine suitability for the procedure.
The first method of percutaneous fistula creation uses heat to fuse the walls of the artery and the vein in the forearm together which creates communication from the artery to the vein, i.e., the fistula. The vessels that are joined in this method are the radial artery and the deep communicating vein.
During this procedure, a vascular specialist will use ultrasound guidance to create a small puncture into the skin and into a superficial vein. The physician then inserts a wire that is advanced distally (toward the direction of your hand) until the wire passes through the superficial vein and punctures the wall of the radial artery. Next, a sheath is temporarily placed between the vein and artery as the wire is removed and a special catheter is inserted. The catheter then pulls the walls of the vein and artery together, while thermal energy is then activated to finalize the connection. (iii)
A second method for percutaneous fistula creation uses radiofrequency energy instead of thermal energy. This method creates the fistula by making a connection between the ulnar artery and ulnar vein in the proximal forearm. The ulnar vessels are run along the inside of your arm, located on your pinky side. (iii)
This procedure uses fluoroscopic guidance instead of ultrasound guidance. Fluoroscopy is an imaging technique that uses X-rays to obtain real-time moving images. A vascular specialist makes a small incision in the upper arm, inserts a dual catheter system into the brachial artery and brachial vein. The catheter is advanced distally until it reaches the ulnar artery and ulnar vein, respectively. Once the catheter is in proper alignment, magnets within the catheter pull the ulnar artery and ulnar vein together and radiofrequency is activated, creating the connection, or fistula, between the two vessels.
Advantages of Percutaneous Fistula Creation
Percutaneous fistula creation is a minimally invasive procedure that requires only regional or local anesthesia with a procedure time of less than 30 minutes. Additionally, because the procedure uses an endovascular (within the vessels) approach, it leaves the vasculature and tissue around the AV fistula undisturbed, improving healing time and overall outcomes. Depending on which percutaneous fistula creation method is used, the patient will be left with one or two small puncture sites as opposed to a lengthy scar common with traditional surgical fistula creation. (iii, iv)
Furthermore, the type of fistula connection made between the vessels during a percutaneous fistula creation has its benefits. An anastomosis is the clinical term used to describe the connection made between adjacent blood vessels. Both of these technologies above create a connection that is known as a “side-to-side” anastomosis because one side of the vein wall is being connected to one side of the arterial wall. Side-to-side configurations are believed to be associated with minimal stress on the vessel walls, less development of wall thickening, and more favorable blood flow characteristics. (iii)
These devices also avoid complications that are associated with surgically created AV fistulas, such as poor incision site healing and vessel clamping and dissection.
Finally, utilizing percutaneous fistula creation has reportedly lower costs secondary to the quicker procedure time as well as the use of local vs. general anesthesia. (iii)
Disadvantages of Percutaneous Fistula Creation
While utilizing a percutaneous approach to fistula creation certainly shows promise for reducing complications associated with traditional surgical fistulas and increasing patient satisfaction, percutaneous devices are still relatively new to the U.S. market. More extensive studies may be required to validate efficacy in a wide range of patients. (iv)
Additionally, several important differences exist in the dialysis process for percutaneous AV fistulas. First, there is no surgical scar to help identify the anastomotic site when placing the dialysis needles. Furthermore, because the configuration of the percutaneous fistula is slightly different than the surgical approach, cannulation location will vary according to development of the superficial outflow veins, requiring individualization of the cannulation technique. (iii) These concerns are likely to lessen as more percutaneous fistulas are utilized, and dialysis specialists gain more experience with this approach.
Who is the Right Candidate for Percutaneous Fistula Creation?
The criteria for percutaneous fistula creation is similar to the criteria for surgical fistula creation. Prior to the creation of any fistula, patients should undergo vessel mapping to determine the size and suitability of the vessels. Patients with vessels less than 2 mm in diameter or those too far apart are not ideal candidates for a percutaneous fistula. Furthermore, if the ultrasound determines that the patient has poor-quality perforating veins, but good cephalic or basilic veins, a surgical fistula may be recommended rather than a percutaneous fistula. (v)
Additionally, if a patient has central vein stenosis—a narrowing or blockage of the deep veins in the neck—a percutaneous fistula is unable to be performed. (v)
Talking to Your Doctor about Percutaneous Fistula Creation
If your doctor has determined that you will need dialysis due to worsening kidney functioning, it is important to work together with your doctor to determine the best type of access for your treatment and if a surgical versus percutaneous fistula creation is right for you.
Sources:
(i) National Kidney Foundation. (n.d.). Hemodialysis Access. Retrieved July 3, 2019 from https://www.kidney.org/atoz/content/hemoaccess.
(ii) Mayo Clinic. (n.d.). Hemodialysis. Retrieved July 3, 2019 from https://www.mayoclinic.org/tests-procedures/hemodialysis/about/pac-20384824
(iii) CJASN. (June 2019) Place of Percutaneous Fistula Devices in Contemporary Management of Vascular Access. Retrieved July 4, 2019 from https://cjasn.asnjournals.org/content/14/6/938.
(iv) Rajan DK, Ebner A, Desai SB, Rios JM, Cohn WE. Percutaneous Creation of an Arteriovenous Fistula for Hemodialysis Access. J Vasc Interv Radiol. 2015;26(4):484-490.
(v) Endovascular Today. (June 2015) Update on Percutaneous AV Fistula Creation. Retrieved July 3, 2019 from https://evtoday.com/2015/06/update-on-percutaneous-av-fistula-creation.