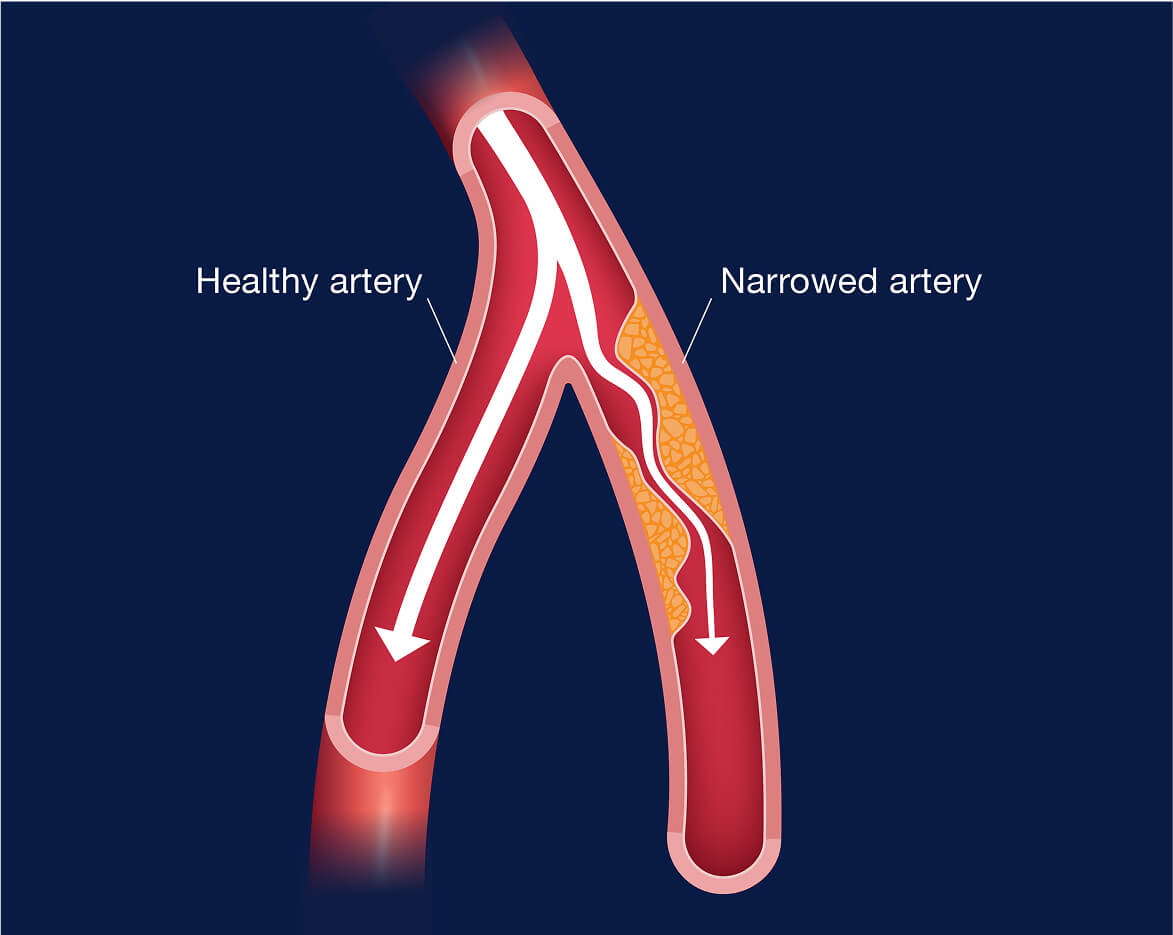
Peripheral artery disease (PAD)
- What is PAD?
- Who is a candidate for PAD procedures?
- What procedures help with PAD?
- What are the benefits of PAD procedures?
Who is a candidate for PAD procedures?
If PAD symptoms are causing you pain or discomfort, then our minimally invasive, nonsurgical procedures could be right for you. These outpatient procedures are quick and offer relief from painful symptoms.
What procedures help with PAD?
If lifestyle changes and medicine aren’t helping, your doctor may recommend angioplasty, stent placement, or atherectomy. These minimally invasive procedures can help restore healthy blood flow and relieve painful PAD symptoms.
PAD is a serious condition, but early detection and treatment may slow down or stop the progression of the disease. Waiting too long or not getting treatment can increase your risk for more serious complications, such as chronic infection or gangrene, and may leave amputation as the only option.
Preparing for a PAD procedure is simple. Your doctor may run tests like a clinical pulse exam, duplex ultrasound, ankle-brachial index (ABI), pulse volume recording (PVR), or computed tomography angiography (CTA) scan to check blood flow and decide the best procedure. These tests are painless. We’ll walk you through every step and are here to answer any questions.
Recovery from a PAD procedure is usually quick. A procedure typically takes less than an hour, and most people go home the same day with just a bandage on their leg. Before you leave, we’ll check for bleeding or swelling. Your doctor may prescribe pain medication and blood thinners—follow instructions closely. Have someone drive you home, avoid heavy lifting for a few days, and stick to light activity. You’ll be back to your normal routine very quickly.
Our centers take most insurance plans. However, always check with your insurance provider to understand what your plan covers and any costs you may incur, such as a co-pay.