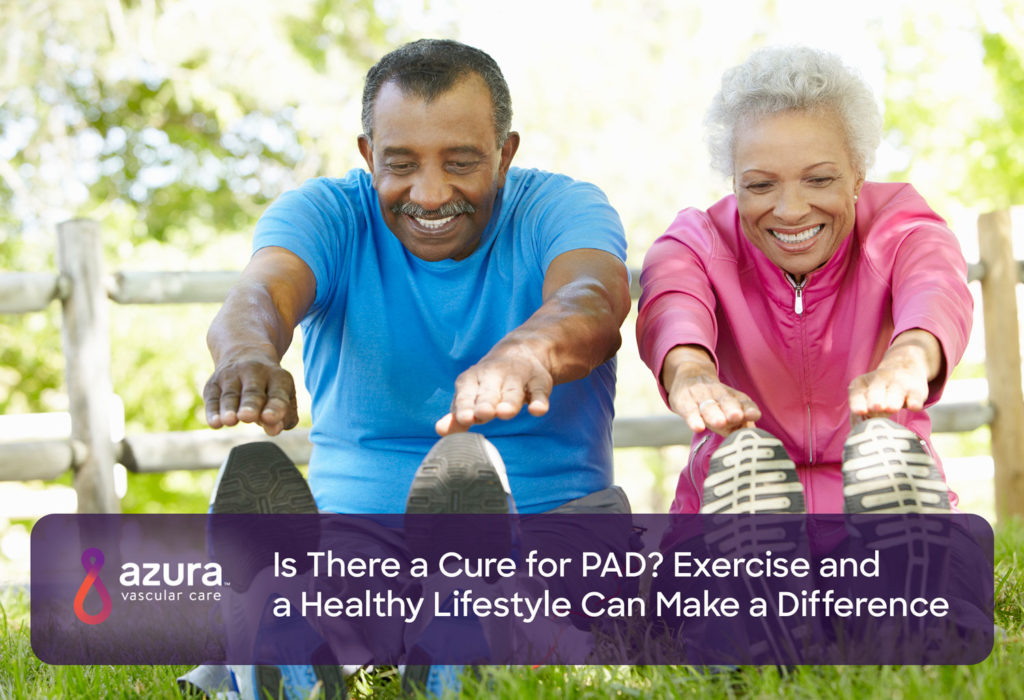
If you’ve been diagnosed with peripheral artery disease (PAD), you’re probably asking yourself, “Is there a cure for PAD?” Unfortunately, when your arteries begin to harden, the process cannot be reversed. There is some good news, however. By making healthy changes to your lifestyle and reducing your high cholesterol level, you can help slow the progression of the disease or prevent your PAD from worsening.
Get Active to Feel Relief
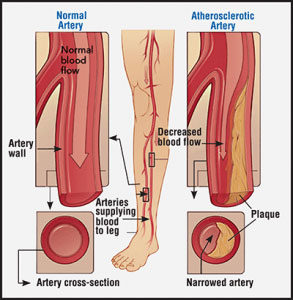
A peripheral artery disease exercise program is recommended for all patients living with PAD, but particularly for those with claudication, or poor circulation in the leg arteries due to plaque buildup. (i) Exercise, combined with lifestyle changes, may slow or stop the progression of PAD. Potential benefits include: (i)
- Reducing limb pain and symptoms
- Improving exercise ability
- Preventing or improving physical disability
- Decreasing the risk of cardiovascular events, such as heart attack and stroke
Although PAD reversal is not possible, regular physical activity can help relieve the symptoms of PAD. (ii) In the beginning, walking may cause pain. However, by alternating activity and rest in timed intervals, you’ll begin to build up the length of time that you can walk before feeling pain. (ii)
Styles of Exercises for PAD Patients
Experts recommend that PAD patients exercise in a monitored environment, like on a treadmill at a cardiac rehabilitation center. (ii) If you aren’t able to go to a cardiac rehab center, your doctor may recommend a community- or home-based program that’s appropriate for your condition. (ii)
If it’s difficult to commit to regular exercise sessions, try to complete at least one 10-minute session of exercise most days. (iii)
Supervised Exercise
 The American Heart Association recommends that patients with PAD participate in structured exercise therapy (SET), which has been shown to produce better results than unsupervised training. (iv, i)
The American Heart Association recommends that patients with PAD participate in structured exercise therapy (SET), which has been shown to produce better results than unsupervised training. (iv, i)
Exercise should be tailored to each patient and should include specific instructions for the type, frequency, intensity, and duration. The most effective structured exercise is conducted in a hospital or outpatient facility. (iv)
Your doctor may clear you for unsupervised exercise if he or she feels it’s safe for you to do so. (i)
Home-Based Exercise for Those Living with PAD
 Research has found that home-based exercise programs, a convenient alternative to supervised exercise, can help those with PAD walk farther and faster. (v)
Research has found that home-based exercise programs, a convenient alternative to supervised exercise, can help those with PAD walk farther and faster. (v)
Speak with your doctor before starting any exercise program. (vi)
Diet Plays a Role in Slowing PAD
Two popular diets make eating healthy easier. These plans have been shown to prevent cardiovascular disease or decrease the progression. (vii)
The Mediterranean Diet
 The Mediterranean diet promotes high proportions of olive oil; legumes, such as peas, beans, and lentils; unrefined cereals; fruits; and vegetables. It also includes moderate to high amounts of fish, moderate amounts of dairy, such as cheese and yogurt, and wine. The plan allows very limited amounts of meat and meat products. (vii)
The Mediterranean diet promotes high proportions of olive oil; legumes, such as peas, beans, and lentils; unrefined cereals; fruits; and vegetables. It also includes moderate to high amounts of fish, moderate amounts of dairy, such as cheese and yogurt, and wine. The plan allows very limited amounts of meat and meat products. (vii)
The DASH (Dietary Approaches to Stop Hypertension) Diet

The DASH diet limits sodium and overall fat intake and restricts alcohol. There is strong evidence this plan reduces hypertension, cardiovascular disease risk, and cardiovascular disease progression. (vii)
By eating a variety of nutritious foods from all of the food groups, you’ll ensure that your body gets the proper nutrients it needs. Be sure to read Nutrition Facts labels and stick to recommended portion sizes.
Before beginning any diet program, it’s important to consult your physician to determine if there are any health issues that may affect you while changing your eating habits.
Smoking and PAD
Smoking is one of the top PAD risk factors, followed by ethnicity, diabetes, poor kidney function, high blood pressure and high cholesterol. (viii)
Smoking increases the risk of developing PAD two to six times, according to the U.S. Centers for Disease Control and Prevention (CDC). (ix)
The strong correlation between smoking and PAD has been the subject of research for more than 60 years (viii). In fact, 50 percent of PAD cases can be directly attributed to smoking. (viii) Additionally, current smokers are almost four times as likely to develop asymptomatic PAD as non-smokers. (viii)
And, it doesn’t take much to up your risk for developing PAD. Smoking even half a pack of cigarettes a day may increase your risk of having PAD by up to 50 percent. (x)
By quitting smoking, you can prevent PAD from worsening and increase your chance of survival. In a recent study, PAD patients who continued to smoke were more than twice as likely to die within five years as those who quit within the year. (xi) Specifically, the risk of dying within five years for the quitters with PAD was 14 percent, compared to 31 percent for those who continued to smoke. (xi)
Patients with extreme PAD who continued smoking were nearly three times as likely to die within five years compared to those who quit. (xi) Specifically, for patients with critical leg ischemia, quitting smoking reduced their risk of dying significantly — from a 43 percent mortality rate within five years for smokers to an 18 percent rate for quitters. (xi)
Living Better with PAD
So, is there a cure for PAD? Unfortunately, PAD reversal is not possible, but by making lifestyle changes like exercise, eating healthy, and not smoking, you’ll greatly improve your health and wellbeing.
Learn more about PAD today. Download PAD Diagnosis and Treatment Options Explained, or call 844-LEG-DOCS (534-3627) to schedule an appointment with a vascular specialist today.
Sources:
i Hamburg, N. M., & Balady, G. J. (2011). Exercise Rehabilitation in Peripheral Artery Disease: Functional Impact and Mechanisms of Benefits. Circulation, 123(1), 87-97. doi:10.1161/circulationaha.109.881888 (accessed April 4, 2018)
ii American Heart Association. Prevention and Treatment of PAD. http://www.heart.org/HEARTORG/Conditions/VascularHealth/PeripheralArteryDisease/Prevention-and-Treatment-of-PAD_UCM_301308_Article.jsp#.WsTs0Zch3IV(accessed April 4, 2018)
iii American Heart Association. The American Heart Association’s Diet and Lifestyle Recommendations. http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/The-American-Heart-Associations-Diet-and-Lifestyle-Recommendations_UCM_305855_Article.jsp#.WsTt9Zch3IU(accessed April 4, 2018)
iv New peripheral artery disease guidelines emphasize medical therapy and structured exercise. (2016, November 13). Retrieved April 04, 2018, from http://newsroom.heart.org/news/x-new-peripheral-artery-disease-guidelines-emphasize-medical-therapy-and-structured-exercise
v American Heart Association. Walking Makes It Better. http://heartinsight.heart.org/Fall-2015/Walking-Makes-It-Better/(accessed April 4, 2018)
vi Penn Medicine. The Best Workout to Manage Symptoms of Peripheral Artery Disease. https://www.pennmedicine.org/updates/blogs/heart-and-vascular-blog/2016/february/the-best-workout-to-manage-symptoms-of-peripheral-artery-disease(accessed April 4, 2018)
vii Cleveland Clinic. Choose the Best Diet for Your Peripheral Arterial Disease. https://health.clevelandclinic.org/choose-the-best-diet-for-your-peripheral-arterial-disease/(accessed April 4, 2018)
viii Action on Smoking and Health. ASH Research Report: Smoking & Peripheral Arterial Disease (PAD). http://ash.org.uk/download/ash-research-report-smoking-and-peripheral-arterial-disease-2/ (Accessed May 10, 2018)
ix Centers for Disease Control and Prevention. Health Effects of Cigarette SmokingPeripheral Arterial Disease (PAD) Fact Sheet. https://www.cdc.gov/DHDSP/data_statistics/fact_sheets/fs_PAD.htm (accessed May 10, 2018)
x Vascular Disease Foundation. Life Saving Tips About… Smoking and PAD http://vasculardisease.org/flyers/lifesaving-tips-on-smoking-and-pad-flyer.pdf(accessed April 3, 2018)
xi Smoking cessation is associated with decreased mortality and improved amputation-free survival among patients with symptomatic peripheral artery disease. Armstrong, Ehrin J. et al. Journal of Vascular Surgery, Volume 60, Issue 6, 1565 – 1571. https://www.jvascsurg.org/action/showCitFormats?pii=S0741-5214%2814%2901630-9&doi=10.1016%2Fj.jvs.2014.08.064 (Accessed May 10, 2018).