Tracing the cause of leg pain can follow many paths. If your leg hurts, you may assume that you have a minor sprain or a pulled muscle. You might also believe that your pain is due to arthritis or a normal sign of aging. But did you know that leg pain is often the first symptom of peripheral artery disease (PAD)? PAD is a potentially serious vascular condition that can have a significant impact on your health. Read on to learn more about vascular leg pain and what steps to take if you think you might have PAD.
What Is Peripheral Artery Disease (PAD)?
Peripheral artery disease is a vascular disorder that affects blood flow to your extremities, most commonly to the legs. The condition is caused by atherosclerosis, the accumulation of plaque material on the inside walls of arteries. (i) Atherosclerosis can prevent your limbs from receiving the oxygenated blood they need. Blocked blood flow can then trigger vascular leg pain.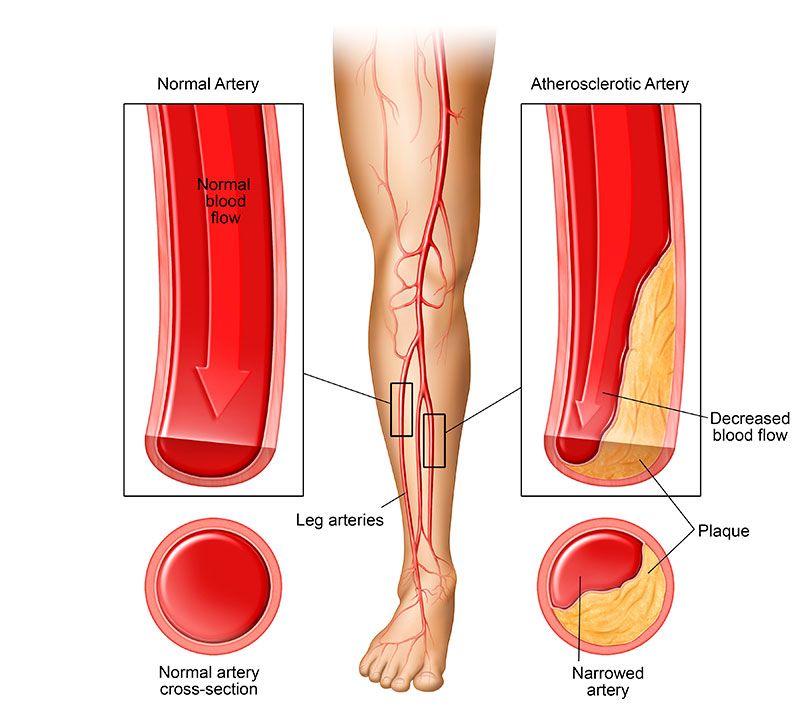
People with early stages of PAD often notice that their legs ache or throb when walking. The pain sometimes disappears with rest but returns the next time you stand or walk. (ii)
PAD is a progressive disease and if left untreated, can have a drastic impact on your health and quality of life. The most advanced form of PAD, known as Critical Limb Ischemia (CLI), can completely block blood flow to the legs. If blood flow isn’t swiftly restored, necrotize. Without intervention and in extreme cases, limb amputation might be necessary. (i)
People with PAD may also develop atherosclerosis in other parts of their body. which can affect blood flow to the heart, brain, or lungs. If you have PAD, you may also be at an increased risk for a heart attack or stroke. (iii)
Symptoms of PAD
PAD is often misdiagnosed since these patients frequently assume that their pain is due to an injury or advanced age. Doctors also sometimes mistake vascular leg pain for an athletic injury or sprain. It’s important to know the signs of PAD so you can advocate for yourself if you suspect you might have this condition.
The most common symptom of a vascular issue is claudication, or leg pain that’s worse with exercise caused by an obstruction in the arteries. (ii) Pain may disappear when you’re resting but return when you’re standing, walking, or climbing stairs. Vascular leg pain often causes a sensation of muscle cramps in the calves. (ii)
As PAD progresses, blood flow to the lower extremities becomes even more limited. If this occurs, you might experience leg pain even when you’re resting or lying down. Leg pain at night can be a sign that your vascular disease is getting worse. (ii)
Other symptoms of PAD include: (ii)
- Muscle weakness
- Numbness in lower legs and feet
- Low temperature in legs and feet
- Sores on legs
- Pale or bluish skin
- Scrapes or wounds of the lower extremities that are slow to heal
- Weak pulse in legs or feet
- Slow growing toenails or leg hair
Leg pain caused by an injury often gets better with time but the pain caused by PAD is often progressive and gets worse without treatment. (iv) Never overlook any kind of long-term pain. Chronic pain or injuries that don’t seem to heal on their own should be evaluated by a doctor.
Other Potential Causes of Leg Pain
Of course, PAD is not the only possible cause of leg pain. Pain in the lower legs and feet can result from a variety of other health conditions, including: (v)
- Muscle strains and sprains
- Torn or ruptured tendons
- Fractures
- Sciatica
- Arthritis
- Bursitis
- Tendinitis
- Herniated disk
Many people also experience lower leg pain due to less serious vascular conditions like varicose veins. (vi) A vascular specialist can evaluate your symptoms and determine if a vascular condition is causing your leg pain.
If you’re diagnosed with PAD, early diagnosis and treatment can help eliminate painful symptoms and prevent life-threatening complications.
RELATED: What Causes PAD?
How Is PAD Treated?
The goal of PAD treatment is twofold: to provide relief from leg pain while also working to stop the progression of the disease.
PAD often requires a complex treatment strategy. Your doctor may prescribe a variety of medications and lifestyle changes (which are indicated below) to address some of the PAD risk factors. These medications, and lifestyle changes can help: (vii)
- Lower cholesterol
- Lower blood pressure
- Control glucose levels
- Prevent blood clots
- Provide pain relief
Maintaining a healthy lifestyle is also an integral part of managing your PAD. Your doctor may recommend a variety of lifestyle changes such as: (vii)
- Quitting smoking
- Following a heart-healthy diet
- Getting more exercise
- Avoiding alcohol
Minimally Invasive Treatment for PAD
Although medication and lifestyle changes can help many patients with PAD, they aren’t always enough to clear blocked arteries. If blood flow to the legs is severely limited, an interventional procedure may be necessary to restore healthy blood flow. A variety of minimally invasive procedures can help with this task. One common procedure for PAD is angioplasty. (vii)
Angioplasty for PAD treatment can be safely and effectively performed in an outpatient setting. During an angioplasty procedure, your vascular specialist threads a thin catheter through your blood vessels into the blocked artery. A balloon on the tip of the catheter is inflated to flatten the built-up plaque against the wall of the artery and improve blood flow. Your vascular specialist may also place a stent to help keep the artery open. (vii)
RELATED: PAD Treatment Options That May Help Your Leg Pain
Don’t Ignore Vascular Leg Pain
It can be tempting to ignore leg aches and cramps. If your legs often hurt, you may tell yourself that aches and pains are a natural part of getting older
Every year, hundreds of thousands of Americans wind up in the emergency room after a heart attack or stroke. (ix) Many had no idea that they were at risk for PAD. Fortunately, early diagnosis and treatment can help preserve your health and clear blocked arteries.
Don’t ignore your symptoms. Take our free PAD risk assessment to learn more about your risk factors and treatment options. Then Call 844-LEG-DOCS (534-3627) to schedule an appointment with a vascular specialist.
Sources:
(i) MedlinePlus. (2018, August 8). Peripheral arterial disease. Retrieved October 22, 2018, from https://medlineplus.gov/peripheralarterialdisease.html
(ii) Mayo Clinic. (2018, July 17). Peripheral artery disease: Symptoms & causes. Retrieved October 22, 2018, from https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
(iii) American Heart Association. (2016, October 31). About peripheral artery disease (PAD). Retrieved October 22, 2018, from http://www.heart.org/en/health-topics/peripheral-artery-disease/about-peripheral-artery-disease-pad
(iv) John Hopkins Medicine. Peripheral vascular disease. Retrieved October 22, 2018, from https://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/peripheral_vascular_disease_85,P00236
(v) Mayo Clinic. (2018, January 11). Leg pain. Retrieved October 22, 2018, from https://www.mayoclinic.org/symptoms/leg-pain/basics/causes/sym-20050784
(vi) Mayo Clinic. (2017, December 28). Varicose veins. Retrieved October 22, 2018, from https://www.mayoclinic.org/diseases-conditions/varicose-veins/symptoms-causes/syc-20350643
(vii) Mayo Clinic. (2018, July 17). Peripheral artery disease: Diagnosis & treatment. Retrieved October 22, 2018, from https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563
(viii) MedlinePlus. (2018, August 8). Atherosclerosis. Retrieved October 22, 2018, from https://medlineplus.gov/atherosclerosis.html
(ix) Centers for Disease Control and Prevention. (2017, November 28). Heart disease facts. Retrieved October 22, 2018, from https://www.cdc.gov/heartdisease/facts.htm