If you or a loved one has recently been diagnosed with a varicocele, or an abnormal enlargement of the scrotal veins, you may be curious to learn more about this diagnosis.
Most likely, your doctor explained to you that a varicocele is a varicose vein of the scrotum caused by incompetent vein valves, resulting in a backup of blood flow from the scrotal veins back towards the heart. When the one-way valves that are present in the veins become weak, blood pools and enlarges the veins in the scrotum, resulting in a varicocele.
Varicoceles may cause pain, swelling or atrophy (shrinkage) of the testicles, and are also the most common diagnosis seen in infertile men.[i] Fortunately, varicoceles are treated by either surgical or minimally invasive procedures.
To help you understand more about the symptoms, effects, and treatments for varicoceles, here is a glossary to help you better understand a varicocele diagnosis.
Glossary
Azoospermia– Absence of sperm in the semen, a potential effect of a varicocele.[ii]
Bilateral Varicocele– A condition that affects both sides of the body; varicoceles occur on both sides of the scrotum. Typically it is more common for a varicocele to occur on the left side.
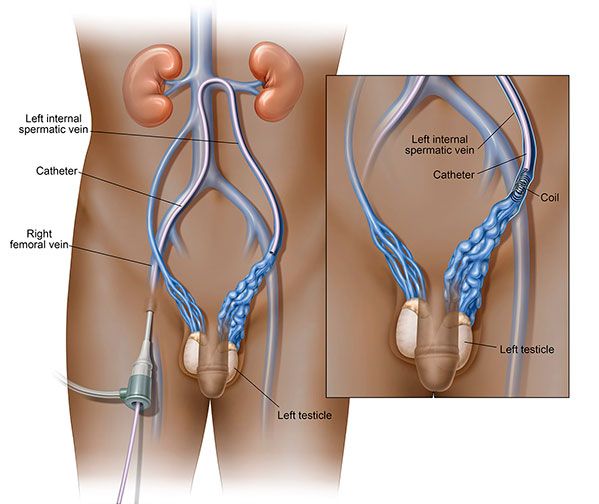
 Coils– Small coils that are made up of stainless steel, platinum, or other medical grade materials are used to directly close off an affected blood vessel during the minimally invasive procedure for varicocele, varicocele embolization. The coils are inserted into the vein that is causing the backflow of blood into the scrotum, and the backflow of blood is diverted to healthy veins, reducing swelling and pressure within the scrotum.
Coils– Small coils that are made up of stainless steel, platinum, or other medical grade materials are used to directly close off an affected blood vessel during the minimally invasive procedure for varicocele, varicocele embolization. The coils are inserted into the vein that is causing the backflow of blood into the scrotum, and the backflow of blood is diverted to healthy veins, reducing swelling and pressure within the scrotum.
DNA Fragmentation – The breaking up of DNA strands into pieces. Varicoceles can cause DNA fragmentation.[iii]
Ejaculation – Ejection of semen during male orgasm. If a man is suffering from a varicocele the amount of, or mobility of the sperm ejaculated may be impacted, resulting in varicocele related infertility.
Follicle Stimulating Hormone (FSH) – FSH is a hormone that is released by the pituitary gland, in men FSH helps to control sperm production. FSH in men should normally remain constant. An elevated FSH level indicates that the varicocele is causing some stress on sperm production.[iv]
General Anesthesia – A form of sedation that affects the entire body, where a patient is completely unconscious. This form of sedation may be used for surgical procedures used to treat varicocele, while only local anesthesia and/ or conscious sedation is used when performing the minimally invasive procedure to treat varicoceles, varicocele embolization.
Hydrocele – A fluid filled sac surrounding a testicle, causing swelling of the scrotum; may be a symptom of a varicocele.
Infertility – The inability to achieve pregnancy after 12 months or more of regular, unprotected sexual intercourse. Varicoceles are the most common diagnosis seen infertile men[i]
RELATED: How Do Varicoceles Cause Infertility and Can it be Reversed?
Jugular Veins – The large veins in the neck that carries blood from the head to the face; also a point of entry for the catheter during the varicocele embolization procedure. Other points of entry include the femoral and basilic vein. Which method is used is based on physician and patient consultations.[v]
Laparoscopic Varicocelectomy – A surgical technique to treat varicoceles, where three small incisions are made in the abdomen, allowing for varicoceles on the left or right to be reached, and clipped and divided. There are two other surgical approaches, open surgery, in this approach the incision is made over the groin and the affected vein is then cut and divided, and microsurgical varicocectomy, where an incision is made in the lower groin and the spermatic cord is isolated, then the veins feeding the varicocele are divided.
Local Anesthesia – The injection or application of an anesthetic to a specific area of the body to prevent patients from feeling pain in that restricted area during medical procedures.
Minimally Invasive Procedures – Minimally invasive procedures, such as varicocele embolization, are performed through small vein punctures and allow patients faster recovery times, and can be performed on an outpatient basis. Patients are generally able to return to normal activities sooner than with surgery.
RELATED: Is There A Minimally Invasive Procedure for Varicoceles?
Oligoasthenospermia – A severely low sperm count and low sperm motility; a potential effect of a varicocele.[vi]
Percutaneous Embolization – Another name for the embolization process, which is used for various conditions. For varicocele, it is the same as a varicocele embolization (see below).
Interventional Radiologist – A physician specially trained in the use of techniques that rely on the use of radiological image guidance (x-ray fluoroscopy, ultrasound, computed tomography, or magnetic resonance imaging) to treat various conditions, including varicoceles.
Sclerosant – A solution that is injected into an affected vein that causes that vein to shrink and dissolve after a few weeks. The body naturally absorbs the treated vein; sometimes used along with or instead of a coil in varicocele embolization.
Testicular Atrophy – a medical condition in which the testicles shrink in size and possibly have a loss of function; may be a symptom of a varicocele.
Urologist – A physician who specializes in diseases of urinary tract and the male reproductive system; can diagnose varicoceles.
Varicocele Embolization – A minimally invasive, outpatient procedure used to treat varicoceles with the use of x-ray image guidance and a catheter. A small coil, and/ or vessel scarring solution (sclerosant) is placed in the blood vessel to block off the blood flow and divert it away from the varicocele and back to healthy veins, relieving pressure, pain and swelling and potentially improving sperm quality.
RELATED: What is Varicocele Embolization?
X- Ray Image Guidance – The use of x-ray imaging to help plan, perform and evaluate procedures. X-ray image guidance is used to visualize the enlarged veins while performing varicocele embolization, the minimally invasive procedure to treat varicoceles.
Hopefully now you have a better understanding about varicocele and its related terms. It helps to know there are treatment options available that can offer symptomatic relief. Remember, there are alternatives to surgery. Find an interventional radiologist in your area who can perform varicocele embolization and set up a consultation to learn more.
Sources:
[i] ASRM Practice Committee. Report on varicocele and infertility: a committee opinion. American Society for Reproductive Medicine and Society for Male Reproduction and Urology. 2014: Vol. 102 No.6 https://www.asrm.org/uploadedFiles/ASRM_Content/News_and_Publications/Practice_Guidelines/Joint_Reports/Report_on_varicocele.pdf
[ii] Pasqualotto FF, Lucon AM, De Goes PM, et al. Induction of spermatogenesis in azoospermic men after varicocele repair. https://academic.oup.com/humrep/article/18/1/108/880401/Induction-of-spermatogenesis-in-azoospermic-men. Hum Reprod (2003) 18 (1): 108-112.
[iii] Agarwal, Ashok, Thomas, Anthony. Infertile Men with Varicocele Have Increased Nuclear DNA Damage in Spermataozoa. https://www.clevelandclinic.org/reproductiveresearchcenter/pub/uronewsv_10_2.pdf
[iv] Pasqualotto FF, Lucon AM, De Goes PM, et al. Semen profile, testicular volume and hormonal levels in infertile patients with varicoceles compared with fertile men with and without varicoceles. Fertil Steril. 2005;83:74–77. [PubMed]
[v] Tay, KH, Martin, ML, Mayer, AL, Macha, LS. Selective spermatic venography and varicocele embolization in men with circumaortic left renal veins. J Vasc Interv Radiol. 2002 Jul;13(7):739-42. [PubMed]
[vi] Benoff S, Gilbert BR. Varicocele and male infertility: Part I.Preface. Hum Reprod Update. 2001;7:47–54. [PubMed]