Are you among the 15% of men who’ve been diagnosed with a varicocele? If you are, you may be wondering if surgery is the right- and only– treatment option for you.[i]
A varicocele is a collection of dilated blood vessels in the scrotum and around the testicles. Some men with varicoceles opt to have surgery to treat infertility and/or pain. Varicoceles play a part in 40% of couples with male factor infertility. Infertility is the inability for a couple to get pregnant after 12 months of unprotected intercourse.[ii]
If you’re considering surgery to treat your varicocele, you should know about the risks. You should also know there is a minimally invasive treatment alternative, varicocele embolization. Varicocele embolization involves the use of x-ray imaging to locate and then block the blood flow that is causing the varicocele. Embolization is non-surgical and has similar success rates as surgery[iii], so before you decide, learn about your options, starting with the top varicocele surgeries and the associated risks.
Varicocele Surgical Options
If you are considering varicocele surgery, you should be aware of the different types of surgical procedures.
- Open varicocelectomy – This approach involves an incision in the inguinal, or groin, region. The surgeon locates the veins causing the varicocele and ties them off.
- Laparoscopic varicocelectomy – This approach involves several incisions made in the abdomen for equipment to be placed, including a specialized scope. Using the scope, the veins that are causing the varicocele are identified and then tied off.
- Microsurgical varicocelectomy – This approach uses the same initial incision as the open approach, however it uses a microscope to locate the veins and tie them off. This procedure is more time intensive than the other procedures.
Varicocele Surgical Risks to Be Aware Of
While all surgeries come with some risk of infection or bleeding, these are the top varicocele surgery risks that you need to know about.
Hydrocele
- This is the development of a collection of fluid within or around the scrotum and occurs because the lymph flow was disrupted during the surgery.
- Hydrocele can become large and, in rare cases, can rupture.[iv]
- It can cause a feeling of pressure in the scrotum, or may be painful.
- Additional surgery may be needed to relieve the hydrocele.
- The risk of hydrocele may be as much as 9% with the open approach, and is less likely to occur with the use of a microscope.[iv]
Injury to your Artery
- Arteries carry blood that contains oxygen and nutrients to the organs, including the testicles. Arteries and veins can be very close to each other in the body and during varicocele surgery, an artery may be damaged.
- The artery that is most likely to be damaged in varicocele surgery is the testicular artery and this could lead to damage of the testicle.
- This can occur up to 12-24% of the time with the open approach.
- The use of a microscope improves the visualization of the blood vessels and, in the microsurgical approach; the arteries are damaged less than 1% of the time.[v]
Anesthesia Complications
- Laparoscopic varicocelectomy requires the use of general anesthesia and the use of a breathing machine because the medications used make the patient completely unconscious. There is an increased risk of confusion and nausea with vomiting after the surgery.
- Open and microsurgical varicocelectomy can be performed with general anesthesia but can also be performed using numbing medication given directly into the skin or an injection into the back to numb the nerves; in this case you may also receive a sedative.
Recovery Considerations
You should also consider how you will feel immediately after the surgery as well as how long it will take before you feel normal again and can get back to your usual activities. It can take 1-2 weeks to recover from varicocele surgery. Sexual intercourse should be avoided for 4 weeks after surgery.
Varicocele Embolization
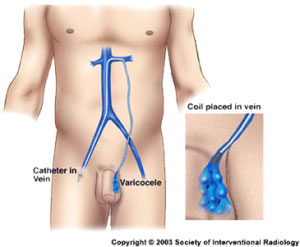 This is a varicocele treatment that does not require surgery. Varicocele embolization is a minimally invasive technique performed by an interventional radiologist. Numbing medication is injected into the skin in the groin and then a catheter, or a thin tube, is inserted into the vein in the leg. Using x-ray imaging, the catheter is advanced into the vein(s) that are causing the varicocele. Once the catheter is successfully placed the affected veins are closed off by the placement of a small coil or coils, and/or the use of a sclerosing agent.
This is a varicocele treatment that does not require surgery. Varicocele embolization is a minimally invasive technique performed by an interventional radiologist. Numbing medication is injected into the skin in the groin and then a catheter, or a thin tube, is inserted into the vein in the leg. Using x-ray imaging, the catheter is advanced into the vein(s) that are causing the varicocele. Once the catheter is successfully placed the affected veins are closed off by the placement of a small coil or coils, and/or the use of a sclerosing agent.
Varicocele embolization is successful about 90% of the time. There is little risk of hydrocele because the lymphatic flow is not disturbed. There is essentially no risk of testicular artery ligation.[iv] Within 1-2 days, you should feel close to normal, and you will be able to exercise within 7-10 days. You can resume sexual intercourse after 1-2 weeks.
Before deciding on a treatment, you should consider all of your options. If you are interested in discussing varicocele embolization, find an interventional radiologist who specializes in this procedure. Review your goals and medical history with the interventional radiologist to determine if varicocele embolization is a good option for you.
Sources:
i Choi, W., and Kim, S., Current Issues in Varicocele Management: A Review. World J Mens Health, 2013. 31(1): p. 12-20. http://wjmh.org/DOIx.php?id=10.5534/wjmh.2013.31.1.12 (accessed 7/31/16)
ii American Society for Reproductive Medicine, Male Infertility. http://www.reproductivefacts.org/topics/detail.aspx?id=1331 (accessed 7/31/2016)
iii Ramasamy, R. (2014). Percutaneous embolization: A viable treatment option for varicocele. Basic Clin Androl, 24(10), 1. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4345412/
iv American Society for Reproductive Medicine, Male Infertility. http://www.reproductivefacts.org/topics/detail.aspx?id=1331 (accessed 7/31/2016)
v Kupis, L., Dobronski, P.A., Radziszewski, P., Varicocele as a source of male infertility – current treatment techniques, Cent European J Urol, 2015. 68: p. 365-370. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4643713/ (last accessed 7/31/2016)