If you’re among the 15% of men who’ve been diagnosed with varicoceles, you probably have a lot of questions about your treatment options.[i]
What Are Varicoceles and Is Surgery Necessary For Treatment?
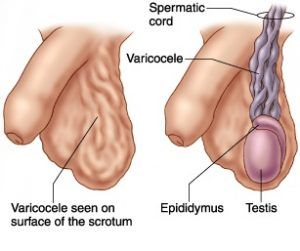
Varicoceles are a collection of veins (blood vessels) which become enlarged, inside the scrotum. They can be asymptomatic in some men, and cause pain and infertility in others. It’s estimated that varicoceles may play a role in up to 40% of couples dealing with infertility, defined as the inability to get pregnant after one year of unprotected sexual activity.[ii] It’s not always the case that a varicocele absolutely needs to be treated, but those who are dealing with pain or infertility may be considering surgery as a form of treatment.
If you’re considering surgery, it’s important to be aware of the complications that can occur as a result. You should also understand how surgery can potentially impact your future fertility.
It is also important to research all of the treatment options available to you, including varicocele embolization. Varicocele embolization is a treatment for varicoceles that is non-surgical, and as a result, does not carry the same risks as surgery.
Learn more about the common varicocele surgery complications below.
Are There Varicocele Surgery Complications I Should Be Aware Of?
When it comes to varicocele treatment, focusing on the benefits, such as possible improvement of fertility, may be easy. But, perhaps more importantly, is looking at whether or not any complications may arise as a result of surgery as a treatment option.
Any surgery has some risk, such as bleeding and/or infection at the incision site. But there are also some major complications specific to varicocele surgery that you should be aware of:
- Varicocele recurrence can be due to incomplete blockage of the veins that are causing the varicocele. This may result in persistent symptoms and problems with fertility.
- Hydrocele formation, or a collection of fluid in or around the scrotum, results from the disruption of the lymphatic flow. Hydroceles can become large and cause pressure in the scrotum. Rarely, one can rupture.[iii] Surgery or drainage may be needed to correct a hydrocele.
- Testicular artery ligation, or the accidental tying off of the blood flow to the testicle, can occur with some surgical approaches. There are concerns that this may result in testicular atrophy and decreased testicular function, such as lower testosterone levels and decreased sperm quality.[iv]
Types of Surgery
There are several different types of surgical approaches for the treatment of varicoceles and each has its own risk of complications.
Open varicocelectomy requires an incision in the inguinal region (groin), in order to access the veins that are causing the varicocele and tie them off.
- Recurrence risk is almost 15%, as not all of the contributing veins may be tied off.[v]
- Hydrocele risk is up to 9% due to disruption of the lymphatic flow because of the location of the surgery.[v]
- Accidental testicular artery ligation risk or injury can vary from 1-12%, depending upon the technique.[iv]
Laparoscopic varicocelectomy involves several small incisions in the abdomen, for the insertion of a scope (camera) and surgical instruments, to access the veins that are causing the varicocele and tie them off.
- Recurrence risk is up to 6%.
- Hydrocele risk is about 2%.
- There is an increased risk of injury to the intestines and major blood vessels with the insertion of surgical instruments into the abdomen. Injuries occur in about 7.6% of cases.[iv,vi]
Microsurgical varicocelectomy uses a microscope to locate the affected blood vessels through an incision in the groin. This approach has the lowest complication rate, but it takes longer to perform than the other surgical approaches.[iv]
- Recurrence risk is 1%.
- Hydrocele risk is 0.44%.
- Accidental testicular artery ligation risk is about 1%.[v,vi]
Fertility
For some men, problems with fertility may be the main reason to seek varicocele treatment. Varicoceles are thought to cause lower sperm production and lower quality of sperm. Correction of a varicocele may lead to increased sperm production and improved sperm quality.i The effect of any procedure on fertility needs to be considered.
- For open varicocelectomy, the pregnancy rate is 33 – 37%.
- For laparoscopic varicocelectomy, the pregnancy rate is 30 – 40%.
- For microsurgical varicocelectomy, the pregnancy rate is up to 50%.[v]
Also Consider Varicocele Embolization – A NonSurgical Option
If you’re worried about the risks associated with surgery, but you want to treat your varicocele, you may be excited to learn that there is a minimally invasive alternative to varicocele surgery. Varicocele embolization is an outpatient procedure, performed by an interventional radiologist and is non-surgical. The procedure uses x-ray imaging to insert a catheter into a vein in your groin to locate the blood vessels leading to the varicocele, and then the veins are sealed off. It is a safe and effective treatment for varicoceles and varicocele related infertility.
- Procedure success is about 90%.
- Hydrocele rarely occurs because the lymphatics are not involved in the procedure.
- Testicular artery injury is unlikely to occur because the arteries are not involved in the procedure.
- The pregnancy rate is approximately 33%.[v]
Keep in mind, every procedure comes with certain risks, so it’s important to discuss your particular situation with your doctor. If you’re interested in discussing varicocele embolization with a specialist, make an appointment with an interventional radiologist who specializes in the procedure. The interventional radiologist will review your medical history and treatment goals in order to help determine if this non-surgical procedure is a good option for you.
Sources:
[i] Choi, W., and Kim, S., Current Issues in Varicocele Management: A Review. World J Mens Health, 2013. 31(1): p. 12-20. http://wjmh.org/DOIx.php?id=10.5534/wjmh.2013.31.1.12
[ii] American Society for Reproductive Medicine, Male Infertility. http://www.reproductivefacts.org/topics/detail.aspx?id=1331 (accessed 7/31/2016)
[iii] Flores V.X., Wallen, J.J., Martinez, D.R., Carrion, R., Deflate-gate: Conservative Management of a Large Ruptured Hydrocele, Urology Case Reports, 2015. 3: p. 198-200. http://www.urologycasereports.com/article/S2214-4420(15)00133-3/abstract (accessed 8/1/2016)
[iv] Zhang, H., Liu, X.P., Yang, X.J., Huang, W.T., Ruan, X.X., Xiao, H.J., Li, L.Y., Gao, X., and Zhang, Y., Loupe-assisted versus microscopic varicocelectomy: is there an intraoperative anatomic difference? Asian J Androl, 2014. 16(1): p. 112-4. http://www.ajandrology.com/temp/AsianJAndrol161112-7640495_211324.pdf (accessed 8/2/2016)
[v] Kupis, L., Dobronski, P.A., Radziszewski, P., Varicocele as a source of male infertility – current treatment techniques, Cent European J Urol, 2015. 68: p. 365-370. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4643713/ (last accessed 7/31/2016)
[vi] American Society of Anesthesiologists, Effects of Anesthesia. https://www.asahq.org/whensecondscount/patients%20home/preparing%20for%20surgery/effects%20of%20anesthesia (accessed 8/1/2016)