While up to 85% of men with varicoceles are asymptomatic, some men do experience symptoms of varicoceles that are potentially problematic. i A potentially serious symptom is when a varicocele causes low testosterone. If you think you are experiencing a dip in your testosterone levels, it is recommended that you speak to a physician. But first, lets learn a bit more about varicocele and testosterone levels?
The Basics of Varicoceles
A varicocele is a varicose vein, or veins, in your scrotum, the pouch of skin that holds your testicles. When these veins, called the pampiniform plexus, stop working correctly, blood can pool in your scrotum, forming a varicocele. This occurs when the one-way valves in these veins malfunction.
Varicoceles and Low Testosterone Levels
Some studies have shown that a varicocele can cause low testosterone levels in some men. ii Low testosterone levels in adolescent boys and men can lead to serious health concerns.
Testosterone is a hormone that is produced primarily in your testicles. It is the primary male hormone and is responsible for regulating male characteristics, including sexual development and sexual function.
When your testicles are not producing enough testosterone, you can experience a number of unpleasant side effects, some of which can lead to serious health concerns and lifestyle issues.
Men with low testosterone levels can experience one or more of the following side effects:
- Decreased exercise tolerance
- Depression

- Fatigue
- Hot flashes
- Increased irritability
- Lack of ambition
- Low energy
- Low sex drive
- Osteopenia or osteoporosis (low bone mineral density)
- Reduced muscle mass or muscle weakness
- Sexual dysfunction
- Trouble concentrating
- Trouble sleeping iii
Do You Think You May Have Low Testosterone?
If you have a varicocele and symptoms of low testosterone, ask your doctor about the link between a varicocele and testosterone levels. If your doctor suspects your testosterone level is low, he or she may order a simple blood test.
There is wide variation in what is considered a “normal” range for testosterone levels. A normal testosterone level can also vary by age. In general, a testosterone level that falls between 300 ng/dL (nanograms per deciliter) and 1,050 ng/dL is considered within the normal range.
If your testosterone level falls below normal and you have a varicocele, your doctor might recommend treatment. In fact, some researchers assert that varicocele treatment can be beneficial for men with a varicocele and low testosterone, even if fertility (which often can be a complication of varicoceles) is no longer an issue. iv If it’s determined that you need treatment for your varicocele, your doctor will likely talk to you about your options: surgery or varicocele embolization.
Surgery Used to be the Only Option to Correct a Varicocele
At one time, surgery was the only option available to correct the faulty veins causing your varicocele. Varicocele surgery is still an option today, but it’s not your only, nor necessarily your best, choice for treatment.
There are three surgical options that can be used to treat a varicocele:
- Open surgery – this option carries a higher rate of varicocele recurrence than other surgical methods. In brief, an incision is made into your scrotum, and the malfunctioning veins are tied off with sutures.
- Microsurgical approach – this approach is performed using a microscope that allows your surgeon to better see the affected veins. This approach has a lower varicocele recurrence rate than open surgery, but it’s a technically complex surgery.
- Laparoscopic approach – this surgery requires you to be put under general anesthesia, and as such, is often not a preferred method to correct a varicocele.
Non-Surgical Varicocele Embolization is an Effective Treatment
Varicocele embolization is a minimally invasive procedure that can be safely performed on an outpatient basis. During varicocele embolization, rather than a true incision, an interventional radiologist only needs to make a small nick in your skin.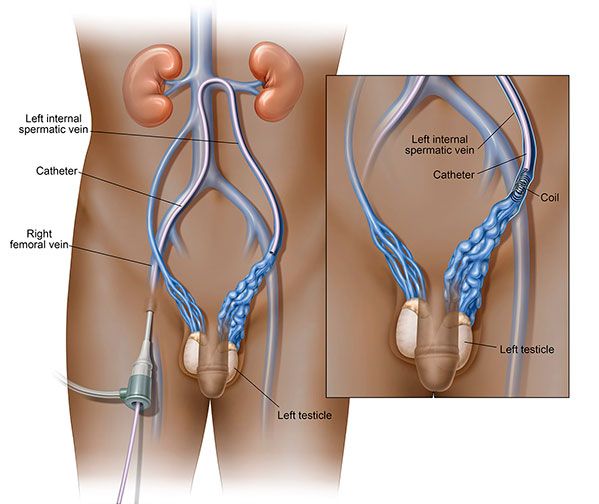
After nicking the skin, typically in the groin area, a small tube, or catheter, is inserted and imaging helps guide the catheter to the affected veins in the varicocele.
Once the malfunctioning veins have been reached, small metal coils, called vascular coils, along with a solution to reduce dilation, are inserted into the affected veins, thereby, blocking them off. This effectively redirects the blood flow out of your scrotal veins into nearby healthy veins and back toward your heart.
Both surgery and embolization are highly successful, about 90%, in treating varicoceles, but men who have had both procedures often prefer embolization. This may be partially due to embolization being an outpatient procedure, almost never requiring hospitalization. v
Advantages to Varicocele Embolization
For many men, there are several advantages to choosing varicocele embolization over surgery, including:
- No additional pain or scarring
- No general anesthesia needed
- No incision, thus no stiches
- Reduced risk of infection or hydrocele (a buildup of fluid around your testicles)
- Shorter recovery time
Some men may not suffer from symptoms of varicoceles and don’t consider treatment. In cases where a varicocele causes low testosterone levels, treatment may be the next best step.
If you have a varicocele and symptoms of low testosterone, talk to an interventional radiologist about a non-surgical treatment option.
Sources:
i Goldstein, M. (2012). Surgical management of male infertility. In: Wein, A., Kavoussi, L. R., Novick, A.D., Partin, A. W., and Peters, C. A. (editors). Campbell-Walsh Urology. Philadelphia: Elssevier Saunders.
ii C. Tanrikut, M. Goldstein, J. S. Rosoff, R. K. Lee, C. J. Nelson, and J. P. Mulhall. (2011). Varicocele as a risk factor for androgen deficiency and effect of repair. BJU International, DOI: 10.1111/j.1464-410X.2010.10030.x
iii Mayo Clinic (2017) Varicoceles. Retrieved from: http://www.mayoclinic.org/diseases-conditions/varicocele/basics/treatment/con-20024164
iv A. Dabaja and M. Goldstein. (2016) When is a varicocele repair indicated: the dilemma of hypogonadism and erectile dysfunction? Asian J. Androl., 18(2). p. 213-216. DOI: 10.4103/1008-682X.169560. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4770488/
v M. Bittles and E. Hoffer. (2008) Gonadal vein embolization: treatment of varicocele and pelvic congestion syndrome. Semin. Intervent. Radiol., 25(3). p. 261-270. DOI: 10.1055/s-0028-1085927. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036435/